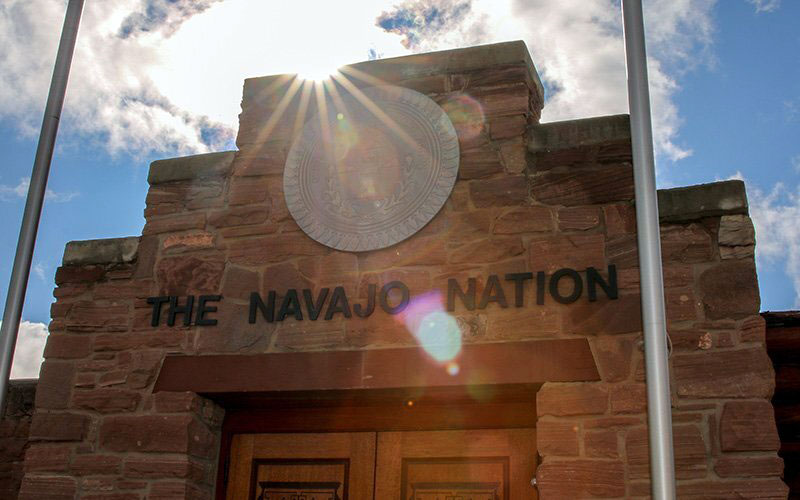
Navajo Nation health officials said hospitals in the region are being stretched to the breaking point by a new surge in COVID-19 cases – 300 on three separate days in just the past week. Unlike earlier this year, there is little outside relief as communities across the country grapple with their own pandemic surges. (File photo by Chelsea Hofmann/Cronkite News)
WASHINGTON – With a shortage of beds, oxygen and staff, the Navajo Nation can no longer depend on regional aid and is sending critical patients farther afield for care, officials reported Thursday.
That news came as area health care workers and Navajo government officials warned that the coming surge in COVID-19 cases would be worse than the first, when the tribe recorded some of the highest infection and death rates in the country.
“It’s gotten to the point where our facilities are deeply challenged and getting to the point of being overwhelmed,” said Dr. Jonathan Iralu, a national and area infectious disease consultant for the Indian Health Service.
“Our hospital beds are full, and when we try to send persons to other hospitals in New Mexico and Arizona … they are essentially 100% full,” said Iralu, who works at the Gallup Indian Medical Center.
His comments came during a wide-ranging two-hour update during which tribal officials said they are extending a reservation-wide lockdown for another three weeks and are seeking a disaster declaration from the federal government.
Navajo Nation President Jonathan Nez said the tribe has also expanded the number of alternative care centers, where people who test positive can “hunker down” and wait out their quarantine period, rather than go home and risk infecting family members. He said the seven alternative care centers will help keep hospital beds open for more serious cases.
Dr. Eric Ritchie, chief medical officer at the IHS hospital in Chinle, said Navajo hospitals “are reaching a breaking point and a point of crisis … both for COVID and for non-COVID care.”
He and others said that the main difference between this surge and the spring is that when reservation and border community hospitals ran out of beds then, they could easily transfer patients to hospitals in Albuquerque or the Valley. But those hospitals are now facing their own COVID-19 crises.
That has put a strain on all medical services for Navajo. Ritchie said a patient recently came to the Chinle hospital in a coma for a non-COVID issue, and it took the staff 24 hours to find a hospital that could accept the patient for the specialized care they needed.
While the shortage of personal protective equipment for hospital staff was a problem in the spring, health care workers now find themselves running short of oxygen and high-flow oxygen machines, one of the primary tools for treating COVID-19 patients.
“We are competing for oxygen supplies,” said Dr. Paula Mora, chief medical officer at the Gallup hospital. “Many of our vendors that provide oxygen for our hospitals are challenged with getting replenished supplies into their companies and therefore we are challenged with trying to find new vendors to provide oxygen.”
Fewer patients require ventilation, but many require “extensive and prolonged oxygen support,” said Dr. Quida Vincent, clinical director at the Northern Navajo Medical Center in Shiprock, N.M. When her hospital had too few high-flow oxygen machines for the number of patients who needed them last week, they made adjustments, “but it was traumatic for staff.”
She expected 10 new machines to arrive Thursday – when workers will need to adapt the new machines to the old hospital, which does not have sufficient oxygen hookups to meet the need she anticipates.
Hospitals are also creating ways to expand bed capacity, but the bigger problem is finding health care workers to staff them. Vincent said there is a 50% nurse vacancy rate, made worse by the spring wave and worker fatigue. All the officials noted that the health care workers they do have are reaching a breaking point.
“Many are disheartened to see the rise in cases and are struggling to come to grips with the fact that we are going to face a moment in time where our hospitals are stretched even further than they were before, during May or June when we had the first surge,” Ritchie said.
At his hospital, Iralu said, “You can see their worry lines on their faces above their face masks.”
Nez said the current public health executive order – which was set to end Sunday – will be extended another three weeks, until Dec. 27. The order mandates a stay-at-home lockdown, closing the Navajo Nation and limiting residents to their homes, with the exception of essential workers and services.
“We need to recommit ourselves to staying home and helping bring these numbers down,” he said.
The new order will allow essential businesses to be open from 7 a.m. to 7 p.m., from Monday through Friday, rather than having to close at 3 p.m. Weekend lockdowns will run from 9 p.m. Friday to 5 a.m. Monday, and people will have to stay home from 8 p.m. to 5 a.m. on weeknights.
“This is entirely in our hands,” said Nez, urging residents to abide by the rules. “We’ve got to encourage and we’ve got to hold our people accountable.”
Vice President Myron Lizer told “negative Nellies out there” that it was time to “fall in line.”
Dr. Michael Tutt, chief medical officer at Tsehootsooi Medical Center in Fort Defiance, said he and his children haven’t seen his elderly parents since February, due to the risk of spreading the virus. At the same time he has “seen grandmothers and grandfathers, husbands and wives die from COVID.”
The Navajo Nation had recorded 17,035 confirmed cases of COVID-19 and 658 deaths as of Wednesday. But Tutt said hope is around the corner.
“There’s a vaccine coming,” Tutt said. “Don’t be afraid of it because you hear all this nonsense on Facebook, on the news.”
After a vaccine comes, he said, “We’ll gather up at our chei’s (grandpa’s) sheep camp and go camping like the way we did in the past.”



