
Scottsdale Recovery Center, where Justin Bronson is a peer support specialist, on April 11. (Photo by Jack Orleans/Cronkite News)
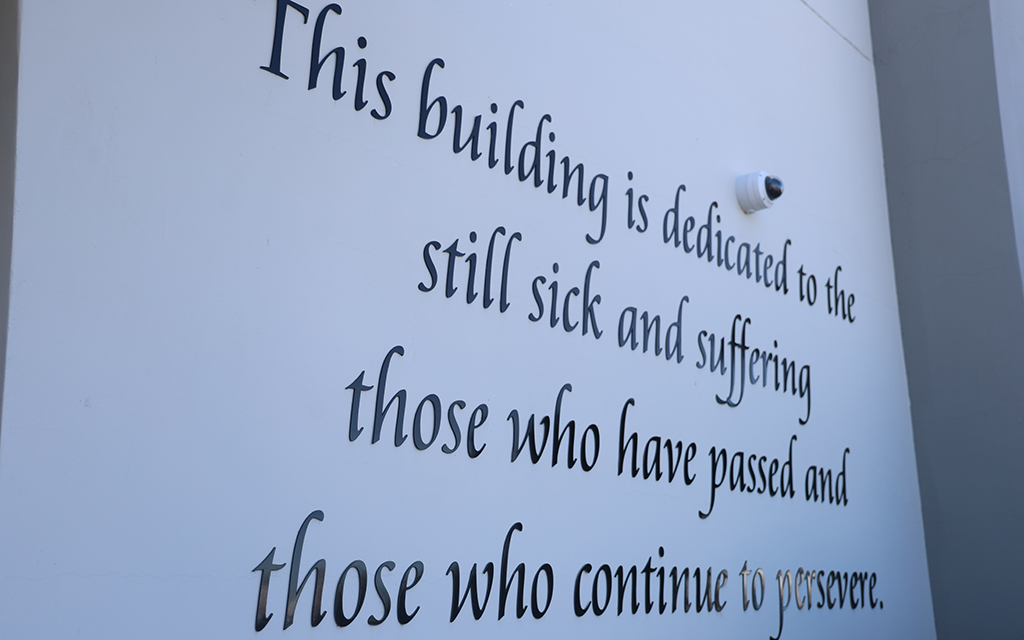
A vignette on the outside wall of Scottsdale Recovery Center on April 11. Scottsdale Recovery Center is one of many addiction treatment centers for people who struggle with substance use problems. (Photo by Jack Orleans/Cronkite News)
PHOENIX – Black people in Arizona die from opioid overdoses more than any other race or ethnicity, according to the Arizona Department of Health Services.
The Opioid Overdoses Surveillance report revealed that Black people in Arizona experience an opioid overdose fatality rate of 32.4 deaths per 100,000 people. Nonfatal overdoses also occur at a higher rate for Black Arizonans than for other groups, at a rate of 67.7 per 100,000 people.
Justin Bronson, a peer support specialist with Scottsdale Recovery Center, an addiction treatment facility, knows the situation well. He remembers witnessing someone near him die from an opioid overdose.
“If I had known what to do, I probably could’ve helped the person, but I didn’t know what to do at the time,” he said.

Justin Bronson is a peer support specialist with Scottsdale Recovery Center. (Photo courtesy of Justin Bronson)
Bronson stressed the importance of having naloxone (branded as Narcan) on hand, a medication designed to rapidly reverse overdose from opioids such as heroin, morphine and oxycodone. It is a temporary treatment that can revive someone in time for emergency personnel to respond.
Bronson also advocates expanding drug education about what to do in situations similar to his and uses his position at the recovery center to help educate the community at large and particularly the Black community.
“I know I could never make up for it because a life was lost, but I feel like I’m helping the next person not be in the same position,” Bronson said.
Bronson, now 39, said he struggled with addiction to cannabis and methamphetamines from the time he was 12 until five years ago. Drug problems put him in prison four separate times on charges including drug possession and robbery before he decided to seek help through a prison drug education class, he said.
The impetus to seek help was when his daughter was taken by the state, he said. Drugs are often abundant in prisons, but he said he chose not to use drugs during his last term in prison because of the education class.
Bronson said stigma can discourage people of color from seeking help for their addictions. According to Damond Gadson, a licensed professional counselor who provides therapy through his firm, ABRA Health, the heavy criminalization of drugs during the crack epidemic that started in the 1980s played a big role in portraying addiction as a Black problem.

Damond Gadson said harsh U.S. drug laws in the 1980s and ’90s were “weaponized” against Black people, making them reluctant to seek help. (Photo courtesy of Damond Gadson)
“Unlike the majority of the American community, the African American and people of color community was really impacted in the late ’80s and early ’90s when there was the crack cocaine epidemic,” Gadson said.
The Substance Abuse and Mental Health Services Administration identified fear of legal consequences as one barrier to recovery in the Black/African American community.
According to a 2022 article in the Harm Reduction Journal, France and the U.S. experienced similar increases in crack cocaine use. Because France prohibits aggregation of racial data, however, it was treated there as a socioeconomic problem instead of a racial problem.
Despite a repressive drug policy approach, France had a publicly funded drug treatment system and harm-reduction services for people who use drugs, according to the Harm Reduction Journal article.
“Being addicted to substances was not treated in the same way that opioid and heroin use is being treated today,” Gadson said.
Gadson pointed to the severe penalties of U.S. laws, such as New York’s Rockefeller drug laws and the nationwide Anti-Drug Abuse Act of 1986, which both imposed mandatory minimum sentences for drug possession.
“So even though that person was addicted and they were seeking help and they needed help, they were criminalized and them seeking help was actually weaponized against them for a reason to send them to prison,” Gadson said.
“I know they’re trying to change (those laws) now, but that stigma of being Black and a drug addict, you’re going to go to prison, was there,” Bronson said.
According to the Pew Research Center, the overdose death rate for Black men in 2015 was 17.3 per 100,000 people – lower than the rate for white and Native American men, but higher than Hispanic and Asian men. By 2020, however, the overdose death rate for Black men had tripled to 54.1 per 100,000 people, the highest of any group. Native American overdose deaths doubled in that period, to 52.1 per 100,000 people, just under the Black rate.

Bronson said stigma impeded his search for care in dealing with his own addictions.
“Once I broke those stigmas, it was more about information. It was more about looking around me and realizing I wasn’t the only one dealing with the things that (only) I thought I was dealing with,” Bronson said.
Participants in a Department of Health and Human Services Office of Minority Health report told researchers they faced considerable stigma in seeking help for substance-use disorders and mental health conditions. The 2022 report identified stigma as negatively affecting many aspects of the lives of people of color, “such as their ability to find housing and employment.”
Victor Armstrong, a vice president for behavioral health with Atrium Health, wrote in a blog for the National Council for Mental Wellbeing about the taboo in the African American community against seeking help for mental health problems.
Armstrong said that seeking help is considered a weakness in the face of survival against historical struggles, and Black people are less likely to seek mental health treatment and more likely to prematurely stop treatment.
One in five Americans live with a mental illness, and one in 25 Americans live with a serious mental illness, according to the National Alliance on Mental Illness.
“I’m not the only one dealing with depression. I’m not the only one dealing with sadness, anxiety, being alone, not knowing who to turn to, feeling hopeless. I’m not the only one feeling like this,” Bronson said.

