WASHINGTON – Arizona started purging people from the pandemic-inflated Medicaid rolls this month, a process that could end up pushing more than 600,000 people off the plan, health officials and advocates said.
The Arizona Health Care Cost Containment System said it is doing all it can to make sure people who are removed from the rolls get coverage elsewhere, such as in the Affordable Care Act marketplace.
Advocates welcomed that effort, but said the disenrollment process still creates uncertainty for recipients and will lead to bigger burdens down the road for providers.
“This is just creating anxiety, first and foremost, among those that currently have coverage and could lose it in the coming weeks and months,” said Dr. Daniel Derksen, director of University of Arizona’s Center for Rural Health. “But it also creates ripples in the clinics, and the hospitals, the health providers, that will have to carry a larger burden of charity care, uncompensated care.”
States had been prohibited from dropping people from Medicaid coverage during the COVID-19 pandemic, even if changes in income or other factors meant the recipient no longer qualified for the program. But Congress in December ordered states to begin checking enrollees’ status and canceling coverage for those who no longer qualified as soon as April 1.
Arizona was one of the first states to start the eligibility review, in February, and was one of five to start disenrolling people this month. AHCCCS said it expects to take a year to work through the rolls and check the eligibility of all 2.5 million people currently in the system.
“We don’t want members to panic and call AHCCCS just because they haven’t heard from us in April. That might not be their renewal date, it might be later in the year,” said Heidi Capriotti, an AHCCCS spokesperson. “We’ve segmented the work from the oldest renewal dates in the continuous enrollment requirement period to the newest.”
Capriotti said AHCCCS is working with the state Department of Economic Security to ease the review process for people in the Supplemental Nutrition Assistance Program – food stamps. That collaboration will allow recipients to “renew both programs at the same time,” she said.
Capriotti also said all members of a household will be considered for re-enrollment at the same time, and that families receiving Children’s Health Insurance Program (CHIP) benefits may be able to keep them, even if they no longer qualify for Medicaid.
“Again, (the state is) trying to streamline this renewal process for members to make it as simple as possible so that they understand when their renewals are coming and what programs they’re being renewed for,” she said.
AHCCCS thinks it can determine the eligibility of about three-quarters of Medicaid recipients simply by checking federal databases, like Social Security. It can then send a letter telling the recipient the agency’s decision on their eligibility, if the personal information in their letter is correct.
Those who can’t be checked that way will get a letter asking for information that could keep them on the plan. About half of those who lose their plans will do so because of ineligibility – being over the income limits or not fulfilling other requirements – and the other half will lose coverage because they failed to update their information on the state’s health care site.
Will Humble, the executive director of the Arizona Public Health Association, said it is common for people to lose their Medicaid because of “bad contact information or lack of a follow-up.” But the sheer size of the coverage rolls now could complicate that already difficult process.
“One of the big issues is, in the Medicaid population, people tend to move a lot, apartments and things like that,” Humble said. “Unless they, the member, updates their address information, then AHCCCS sends a letter to their old apartment, and then when they don’t respond, they get kicked off.”
AHCCCS is encouraging recipients to make sure their contact information is current, and to keep an eye out for correspondence from the agency so they can respond. Recipients will have 30 days to respond. If they don’t respond in that time, they would be disenrolled, but would have another 90 days in which they could apply for reinstatement.
Those who do lose Medicaid coverage can be transitioned into coverage through Obamacare, said Morgan Finkelstein, the state director for the Arizona chapter of Protect Our Care. Marketplace enrollment, typically open only from November to January, will be open through July 2024 to accept those kicked off Medicaid.
“I mean otherwise, what would people do if they don’t have any coverage? And going without health insurance is not safe,” Finkelstein said. “I think as long as folks are proactive about making sure their contact information is up to date, there really shouldn’t be an issue.”
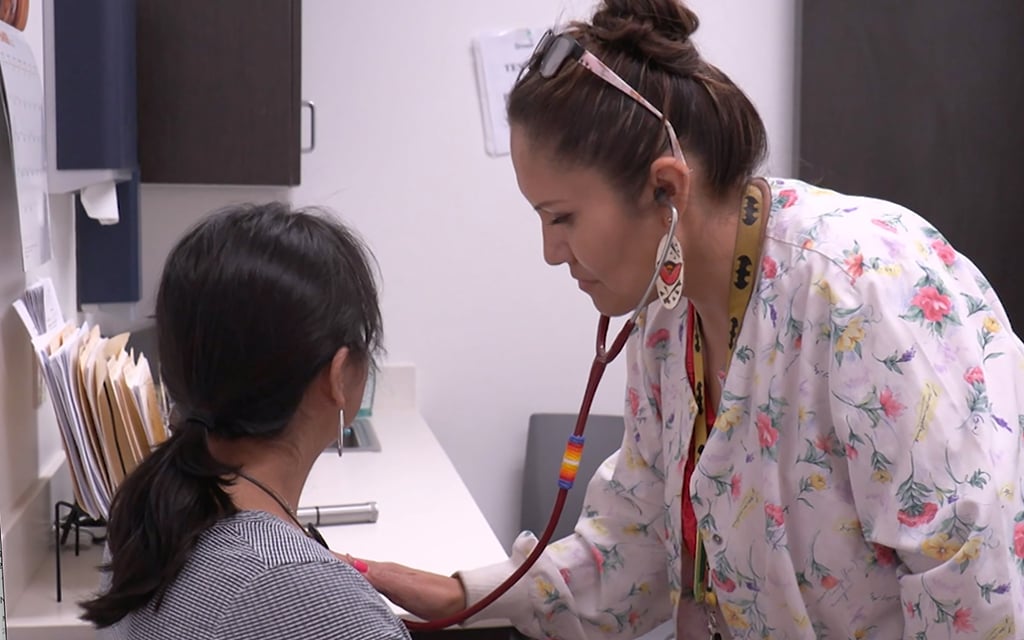
Derksen said people with limited English, with disabilities or who live in rural areas could face the most barriers in keeping access to health care, and that Black, Hispanic and Indigenous people are also likely to be hard hit.
“It’s populations that have been disproportionately affected by the COVID pandemic and also tend to have fewer resources to really respond to these types of things,” he said.
But Capriotti said AHCCCS is working with a variety of community groups to make sure enrollment information is inclusive and accessible.
“We’re trying to find all the different avenues where people interface within their communities and who they trust to get this information from,” Capriotti said. “A lot of people probably don’t trust the government, but they’ll trust their primary care provider or they’ll trust their pastor or their teacher.”
Despite the potential complications, Derksen said community health centers have made “good-faith efforts” to prepare for the end of the public health emergency, a “really important time” for the state’s Medicaid users.
“They (health care providers) really don’t want that fiscal obstacle to be getting in the way of, you know, the care that people need and the preventive services that they should get to prevent things like hospitalization, emergency department visits and things like that,” Derksen said.