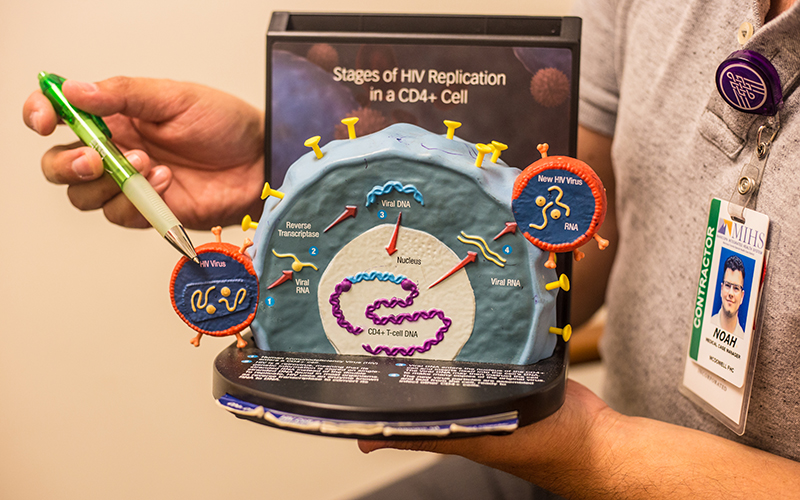
Altman explains how HIV enters the cells of the body and replicates, spreading the virus throughout the body and destroying the immune system. “HIV, when it first started, was referred to as GRID (Gay Related Immune Deficiency). Nobody was talking about the disease because it was a gay disease. HIV is not discriminating. Gay, straight, black, white, young and old can get the disease,” Altman said. (Photo by Lerman Montoya/Cronkite News)
PHOENIX – When Noah Altman moved from Yuma to Phoenix in 2010, he finally felt at peace. He suddenly went from a small border town to a city where there was “gay everything!”
This included a gay Denny’s, affectionately known within Phoenix’s gay community as “Jenny’s,” at Camelback Road and Seventh Street, along with gay bars, sports teams and choirs.
Growing up in Yuma with a Republican father, a religiously conservative Mexican mother and a brother who was his most feared bully, Altman was determined to move to a big city to find his purpose. After receiving his associate degree in general studies at Arizona Western College, he wanted to pursue his bachelor’s degree in Phoenix. He had already arranged to live with one of his closest friends, Whitney, and her mother in the Phoenix area. He didn’t have a job and wasn’t going to school yet, but the then 21-year-old started volunteering at the Phoenix Pride Center downtown.
Altman vividly remembers one Thursday night in February.
The center was offering free rapid-response HIV testing for LGBTQ people. As young men and women patiently waited to hear their results, Altman realized he had never been tested before. He had been sexually active for a couple years in Yuma, but said he was too afraid and confused to get tested.
“Coming from Yuma, I didn’t know what my resources were,” Altman said. ” I thought HIV/AIDS was a nebulous thing that was not affecting me, so I didn’t seek it out.”
That night he got tested. The volunteer was direct: “You are HIV positive.” All he remembers afterward is driving home, completely in shock, tears rolling down his face. He had been in Phoenix less than a month and now, his life was completely changed.
Sex, let alone HIV/AIDS, was a topic Altman rarely considered. Living with his conservative family and lacking an inclusive sex education in school left him vulnerable and clueless when navigating gay sex, he said.
“All I knew about HIV/AIDS was what I learned in the history books,” Altman said. “I learned that I would die.”
Arizona is one of 18 states that do not mandate sex education in public schools, leaving it up to individual districts to decide whether to offer it.
Teresa Simone, community sexuality educator at Planned Parenthood of Arizona, believes the lack of inclusive sex education is leading unknowing young people to partake in risky and potentially life-threatening sexual behavior.
A report from the Journal of Adolescent Health, a peer-reviewed medical journal covering adolescent health and medicine, describes “abstinence only until marriage” (AOUM) programs as inefficient and unethical.
The authors of the report describe AOUM programs to be “coercive, withholding information needed to make informed choices and promoting questionable, inaccurate and stigmatizing opinions.”

Teresa Simone, the community Sexuality Educator at Planned Parenthood Arizona, believes sex education should be more inclusive for LGBTQ students. “We need to give youth across Arizona the tools to practice safe sex. Without any form of sex education, their lives are at risk,” Simone said. (Photo by Lerman Montoya/Cronkite News)
Simone echoed those concerns about abstinence-based programs in Arizona.
“We have seen time and time again, abstinence does not work for adolescent youth,” Simone said. “Youth should be allowed to have access to all the information they need to be safe and healthy.”
Altman’s school in Yuma did provide him with two hours of sex education, but he said it lacked depth and left the students more confused than when they started the class.
“I remember being in health class in high school, and you’d think a semester-long class about health you’d be talking about the human body. I remember we discussed STDs for one day and all they did was show us pictures of rotting penises and rotting vaginas and told us, ‘Don’t have sex because this is what can happen to you.’ ”
Using fear to promote abstinence is common in Arizona public schools, Simone said, and if schools choose to incorporate sex education into their classes, an abstinence-only curriculum is highly stressed.
Discussing HIV/AIDS in Arizona public schools also comes with government restrictions that Simone believes fail to give LGBTQ students a foundation of information in order to have healthy and safe sex.
“There is no mandate for sex education, let alone HIV education in Arizona,” Simone said. “But if a school decides to begin a curriculum of sex education and wants to include HIV preventative methods, schools are not allowed to talk about homosexuality in terms of a positive lifestyle or promote any form of homosexual safe sex options.”
Simone is describing what are known as “no promo homo” laws, a series of local and state laws that forbid public school teachers of health or sexuality education from discussing homosexuality and transgenderism in the classroom.
Under Arizona education law, public school teachers are forbidden to promote a homosexual lifestyle, portray homosexuality as a positive alternative lifestyle and teach safe methods for homosexual sex.
State Sen. Martin Quezada, D-District 29, filed a bill in 2016 to amend that section of the Arizona Revised Statutes, which he believes is homophobic. LGBTQ students deserve equal and inclusive sex education in the state, he said.
“We want to adopt a more comprehensive sex-ed curriculum,” said Quezada,. “I think it’s common sense that we provide kids with information to be healthy adults, regardless of their sexual identity.”
Allowing teachers to talk about safe sex practices and disease-prevention methods, Quezada said, would dramatically reduce teen pregnancies and diagnoses of HIV in young people around the state.
According to data from the Arizona Department of Health Services, there were 147 newly reported HIV cases for ages 13-24 in 2016. That’s a slight increase from the 141 in that age group reported in 2015.
“We live in a fantasy land where we believe that kids won’t engage in sexual activity, so if they’re going to do it, let’s give them the tools they need to do it safely,” Quezada said.
His bill has 14 other Democratic state senators and representatives co-sponsors, but they haven’t been able to advance it out of the Senate Education Committee.
“I introduced the bill in 2016 and it never got a hearing. I have introduced it every year since then and it still hasn’t been heard,” Quezada said, adding that he’ll push for it as long as he’s in office.
Planned Parenthood’s Simone said inclusive sex education in Arizona not only would decrease the number of people diagnosed with sexually transmitted diseases, it could lead the way to end the stigmatization around HIV/AIDS.
Noah Altman said he has experienced that stigma after coming out to close friends and family over the years.
The night he was diagnosed, Altman shared the news with his best friend, Whitney, and her mother. Still in shock and crying in their arms, all he could think about was the death sentence, in his mind, that he had just been given. He got through the next week feeling he was lucky to at least have a place to call home.
But that changed when Whitney and her mother, people he considered family, told him he had to find a new place to live. They feared getting HIV by sharing a toilet.
“The people I loved the most were trying to oust me from their home,” Altman said.
Their reaction highlights the misconceptions and ignorance that still exist when it comes to HIV/AIDS. Some people believe HIV can be transmitted by kissing, touching and even sharing a toilet with someone who’s HIV positive.
For someone to contract HIV – the human immunodeficiency virus – the pathogen must enter the bloodstream through infected bodily fluids, such as blood, semen, vaginal fluids or breast milk. Once in a human host, HIV targets T helper cells, a type of white blood cell that’s fundamental to the immune system.
Instead of attacking, HIV attaches to the white T-cells and transfers the virus. The T-cells do not recognize HIV, causing it to replicate at an astounding rate, spreading the virus throughout the bloodstream. If not treated, HIV kills off the white T-cells it has infected and leaves the immune system deficient of protective cells.
At this stage, HIV turns into AIDS – acquired immunodeficiency syndrome. With AIDS, the immune system is compromised and the patient is now at a higher risk of getting cancer as well as diseases he or she might normally fight off. Patients don’t die of AIDS, they die when the body can’t defend itself from something as simple as a cold.
At the time, Altman did not know the specifics of HIV and believed his diagnosis had put him on a fast track to the grave.
“I was scared because I didn’t know what to do,” he said.
The volunteers who tested Altman wound up helping him secure a place to live. It was with an older gentlemen, also HIV positive.

“I am not ashamed of being HIV positive anymore. It has taken a long time and work for me to love myself and continue with my life,” Noah Altman said. (Photo by Lerman Montoya/Cronkite News)
This person mentored Altman, taking him to his first doctors visit and letting him stay at his home until he was able to get back on his feet and find his own space.
“He didn’t want me to go through what he went through,” Altman said. “He was also diagnosed positive at a young age, and it kind of took him into a spiral of negativity where he fell into drugs, and he didn’t want the same for me.”
Before the introduction of medication used to treat HIV/AIDS, known as antiretroviral therapy, depression and suicide rates among gay men in particular were very high. Now, almost 20 years after the introduction of medication, 22 percent of the people who have been diagnosed with HIV also have been diagnosed with depression.
A report from the peer-reviewed medical journal JAMA Psychiatry, found that depression among people with HIV/AIDS has led to missed medical appointments, inconsistency in medicine intake, detectable viral loads and early death.
“Depression was something I had to battle with,” Altman said. “I think every HIV positive person has experienced a sense of self-hate and regret. There was a time when I stopped taking my medication and didn’t want to go to the doctors. I didn’t like the daily reminder of living with HIV. It took a guy that I was seeing to tell me that I needed to take care of myself for me to get out of that slump and continue fighting.”
HIV/AIDS specialists recommend that diagnosed patients consistently take their medication to lower the viral load, which is the virus amount within the body.
If antiretroviral therapy is continued, the medication can successfully decrease the viral load to levels so low that an HIV test can’t detect the virus. This is called an undetectable viral load.
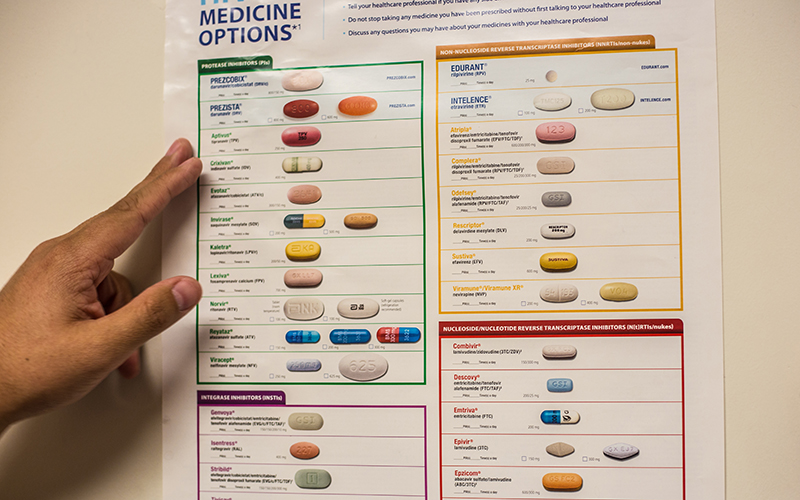
There are approximately 45 different types of HIV medication approved by the Food and Drug Administration that are used for Antiretroviral Therapy (ART). Life expectancy for HIV positive people can be attributed to the effectiveness of ART. In Arizona, less people are dying from the effects of HIV/AIDS. (Photo by Lerman Montoya/Cronkite News)
The Phoenix Indian Medical Center is one of the facilities in metro Phoenix that has received recognition for its work with HIV/AIDS patients. In March, the center was honored for its efforts in HIV viral suppression, reaching the highest mark for any racial group in Arizona. PIMC has received the honor every year since 2014.
The center’s director, Constance James, said Native Americans in Arizona are determined to control the spread of HIV/AIDS in their community.
“PIMC provides care to approximately two-thirds of Native patients living with HIV in Arizona, and those patients achieved a 93 percent viral suppression rate,” she said. “An incredible feat when we see that in 2014, the viral suppression rate in the U.S. among all races for those with an HIV diagnosis was 58 percent.”
She believes the multiple layers of support within the Native American community and Indian Health Service, a federal agency, have been key factors to the success.
“People living with HIV, who take HIV medications daily as prescribed, and achieve and then maintain an undetectable viral load for at least six months, have effectively no risk of sexually transmitting the virus to an HIV-negative partner,” James said. “PIMC has led the way in making this a reality for Native Americans living with HIV.”
This strategy is known as “Treatment as Prevention.”
The Centers for Disease Control and Prevention released a statement last year boasting the effectiveness of antiretroviral therapy, known as ART, in suppressing the viral load.
Despite success in HIV treatment, HIV-positive people continue to be stigmatized.
In response, the U=U campaign, or Undetectable Equals Untransmittable, was created to show that people can live with the virus and still be members of the community and safely have sex without transmitting the virus.
And with the introduction of powerful HIV/AIDS prevention medications, HIV-negative people can drastically limit their chances of contracting HIV.
One of the most popular HIV/AIDS prevention methods for sexual is pre-exposure prophylaxis, most commonly known as PrEP.
PrEP was approved in 2012 by the Food and Drug Administration and is one of the first HIV prevention strategies that can be used by men and women. PrEP comes in the form of a pill that is taken daily to prevent HIV from multiplying and spreading within the body.
The Centers for Disease Control says taking PrEP daily reduces the risk of getting HIV through sex by more than 90 percent. Among people who inject drugs, it reduces the risk by more than 70 percent, according to the CDC.
Through the effectiveness of ART, people with HIV are living longer.
According to data from the Arizona Department of Health Services, 17,464 people were living with HIV, including 780 who were newly infected. Health Services representatives credit advancement in medical treatment with improving survival rates, which are reflected in the number of people living with HIV/AIDS.
After getting on medication and finding his own place to live, Altman said he finally felt ready to focus on what he came to Phoenix to do: Live.

Altman works as a medical case manager at the McDowell Healthcare Center. His patients are mainly homeless or lack stable housing, and many of them also suffer from mental health issues. “If someone is homeless and they’re HIV positive, finding a place to stay the night sometimes takes precedence over making it to their doctor’s appointment or taking their medication,” Altman said. (Photo by Lerman Montoya/Cronkite News)
His HIV diagnosis gave Altman a new purpose in life. He started volunteering and working for the Southwest Center for HIV/AIDS in Phoenix, assisting other gay men who are HIV positive.
He also pursued his bachelor’s degree in social work, knowing he wanted to keep working with people with HIV/AIDS and help them navigate the tumultuousness of the diagnosis. Altman is now a case manager at the McDowell Health Center for high risk patients, some of them battling homelessness and mental health issues.
Since his diagnosis in 2010, Altman has continued to live a healthy lifestyle and has kept his viral load to an undetected status.
“It’s crazy to think that I went from patient to medical-case manager for people living with HIV/AIDS. I had no idea this is where my life was going to lead me.”
