At the federal level, some steps have been taken to help.
Before the pandemic was declared in March 2020, federal law prohibited doctors from prescribing controlled substances without an in-person evaluation. That month, the DEA put the policy on hold for the duration of the pandemic, and specifically allowed doctors to prescribe medications to treat opioid addiction via the internet or telephone.
States also were granted the flexibility to allow opioid treatment programs to prescribe up to 28 days of take-home medication. Usually, patients on medication-assisted treatment are required to visit a facility daily to receive doses and counseling.
President Joe Biden is requesting $10.7 billion from Congress to support medication-assisted treatment, more research and additional behavioral health providers, with an emphasis on assisting Native Americans, older people and rural populations.
But more is needed to reverse the damage done during the pandemic, said Josephine Korchmaros, lead researcher for a University of Arizona program that aims to route people with opioid use disorders into treatment facilities instead of jail.
Even positive steps, such as more providers using telehealth to reach those with substance use disorders, come with roadblocks, Korchmaros said, noting that most of those she serves don’t have consistent access to phones and computers.
“Drug addiction has evolved with all of the additional stressors that come from the pandemic … and the stress and panic that come along with that,” she said.
“People cope with those feelings differently. Turning to substances is just one way.”
Dual crises prompt change
Since its founding in 1983, Scottsdale-based Community Medical Services has sought to help those struggling with drug addiction. Today, the company operates more than 40 clinics in nine states, including a 24/7 “opioid treatment on demand” center in Phoenix that serves about 300 people a day.
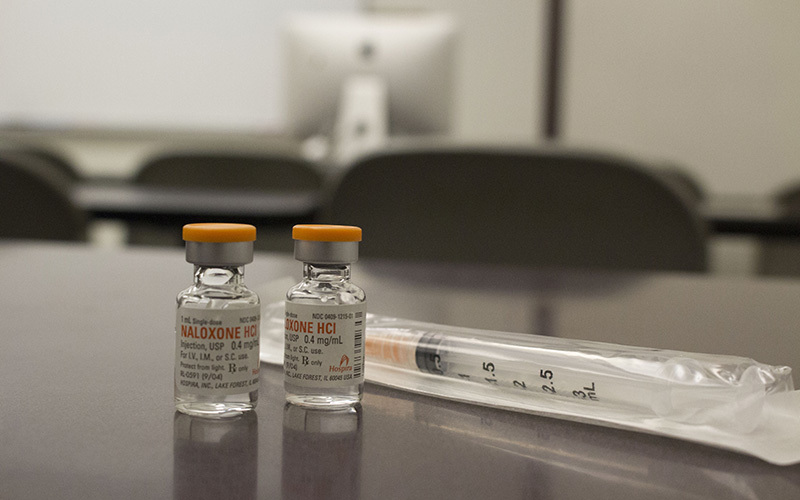
That clinic provides all three government-approved medications for opioid addiction treatment – buprenorphine, methadone and naltrexone – along with counseling and help with employment and housing.
During the pandemic, the clinic’s doors have stayed open, even if operations have a decidedly different look.
Before March 2020, patients would walk in and get evaluated, face-to-face, by a doctor. Those who were prescribed medication were required to report to the clinic daily to take it, and to participate in therapy sessions.
“We get them in right away, no questions asked,” said Jennifer Mason, vice president of operations, “because we know that the next time they use could be their very last.”
Since the beginning of the pandemic, the clinic’s mantra has been “minimizing contact, not care,” Mason said.
Now, patients are ushered into a room and evaluated using video chat on an iPad by a doctor one room over. Waiting room chairs are spaced out for social distancing, and clear shields have been added to the pickup windows where medications are distributed.
Before the pandemic, about 20% of patient interactions companywide were conducted online. By May 2020, that climbed to 88%, Mason said.